The Silent Threat: Why Bangladesh Must Act Now on Zika Surveillance and Testing
Zika virus, once a rarely discussed tropical disease, made global headlines in 2015 and 2016 when it caused a widespread outbreak in Brazil. The virus, primarily transmitted by Aedes mosquitoes, the same type responsible for spreading dengue and chikungunya, raised serious concerns due to its link to birth defects and neurological disorders. Although Bangladesh has never officially reported a large-scale outbreak of Zika, the risk remains very real. With the country’s tropical climate, high population density, and recurring dengue epidemics, an important question arises: Is Zika silently spreading in Bangladesh? The situation calls for urgent nationwide efforts in surveillance, testing, and public health preparedness.
What is Zika Virus?
Zika virus is a type of flavivirus that is mainly transmitted to humans through the bite of infected Aedes mosquitoes. These are the same mosquitoes that spread dengue and chikungunya. The virus was first discovered in 1947 in a rhesus monkey in the Zika Forest of Uganda, and the first human case was identified a few years later. For decades, Zika remained relatively obscure, with only sporadic cases reported in parts of Africa and Asia. However, in recent years, it has emerged as a global public health concern.
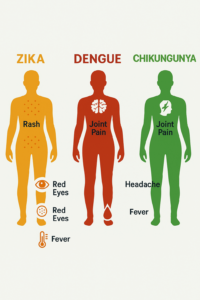
In most cases, Zika virus causes mild symptoms or no symptoms at all, which makes it difficult to detect and control. When symptoms do appear, they typically last for two to seven days and may include:
-
A mild fever
-
A red rash, usually beginning on the face and spreading
-
Muscle and joint pain, especially in the hands and feet
-
Red or irritated eyes (conjunctivitis)
-
Headache and general discomfort
Although the illness is generally mild, the real danger lies in the serious complications associated with Zika infection:
-
Congenital Zika Syndrome: When a pregnant woman is infected with Zika, the virus can be passed to the fetus. This may result in severe birth defects, including microcephaly, a condition where the baby’s brain and head are smaller than normal, leading to developmental delays and lifelong disability. Other complications may include vision and hearing problems, seizures, and limb deformities.
-
Guillain Barre Syndrome: Zika infection has also been linked to Guillain Barre Syndrome, a rare but serious autoimmune condition that causes the body’s immune system to attack the nerves. This can lead to muscle weakness, paralysis, and in some cases, long term disability.
Zika can also be transmitted through sexual contact, blood transfusion, and from mother to child during childbirth. Because of its subtle symptoms and ability to spread in multiple ways, it poses a silent but significant threat in regions where mosquito control and surveillance are weak.
Why Bangladesh is Vulnerable
Although Bangladesh has not seen a major outbreak of Zika, several environmental, social, and systemic factors make the country highly susceptible. With the same mosquitoes that spread dengue already thriving here, and weak health monitoring systems in place, Zika could silently spread without being detected until it is too late.
Presence of Aedes Mosquitoes
Bangladesh is home to both Aedes aegypti and Aedes albopictus, the primary carriers of Zika virus. These mosquitoes are already responsible for recurring dengue and chikungunya outbreaks. Their abundance in both urban and rural settings, particularly in water-filled containers and construction sites, increases the risk of Zika transmission at any time.
Favorable Climate
Bangladesh’s warm and humid weather, especially from April to October, creates ideal conditions for mosquito breeding. Seasonal floods, monsoon rains, and stagnant water bodies further help mosquito populations thrive, increasing the likelihood of Zika spreading if introduced into the population.
Urban Crowding and Poor Sanitation
Major cities like Dhaka, Chittagong, and Narayanganj are densely populated, with limited access to proper drainage, waste disposal, and clean water. These conditions provide countless breeding grounds for mosquitoes and make vector control efforts extremely difficult. Poor housing and informal settlements only add to the challenge.
Weak Disease Surveillance Systems
While health authorities actively monitor dengue outbreaks, Zika remains largely ignored. There are very few diagnostic facilities capable of identifying Zika, and limited public awareness means that mild or asymptomatic cases may go unreported. This gap in surveillance allows for silent transmission.
Travel-Related Infections
Bangladesh has a large migrant population working abroad and strong international trade links. This makes the country vulnerable to imported cases of Zika, especially from regions where the virus is already present. A single undetected case could spark local transmission if the conditions are right.
Has Zika Been Found in Bangladesh?
Yes, Zika virus has been detected in Bangladesh, and recent findings suggest it may be silently circulating. The first sign came in 2014 when International Centre for Diarrhoeal Disease Research, Bangladesh (ICDDR) found Zika antibodies in a local patient. In 2016, the World Health Organization confirmed one official case. However, limited surveillance and the virus’s mild or asymptomatic nature meant that most cases likely went undetected, raising the possibility of ongoing but unnoticed transmission.
In 2023, icddr,b scientists identified the first local Zika cluster in Dhaka’s Mohakhali area. Five patients tested positive, all living within a one-kilometer radius and showing symptoms within a month of each other—strongly indicating local transmission. One patient was co-infected with dengue, a first for Bangladesh. Genetic sequencing confirmed the strain belonged to the Asian lineage, associated with neurological risks like microcephaly. These findings highlight the urgent need for expanded surveillance, testing, and public awareness to prevent a potential health crisis.
The Testing Gap: Why We’re Flying Blind
One of the biggest challenges in identifying and controlling Zika virus in Bangladesh is the lack of adequate testing and diagnostic infrastructure. Zika often presents with mild, nonspecific symptoms such as fever, rash, and joint pain—symptoms that closely resemble those of dengue and chikungunya. As a result, many Zika cases are misdiagnosed or dismissed as more familiar mosquito-borne illnesses.
The problem is compounded by the fact that most public hospitals in Bangladesh do not have the capacity to test specifically for Zika virus. While dengue testing has become more routine due to regular outbreaks, Zika-specific testing remains rare and limited to a few specialized research or private laboratories.
Adding to the difficulty is the lack of multiplex testing kits—advanced diagnostic tools that can detect multiple viruses, such as dengue, chikungunya, and Zika, from a single sample. Without these, doctors often have to rely on trial-and-error testing or clinical judgment, which increases the chances of missing Zika entirely.
Another serious gap lies in medical training and awareness. Many healthcare workers are not fully informed about when to suspect Zika or how to proceed with testing, especially in pregnant women or returning travelers from high-risk areas. This results in underreporting and mismanagement of possible Zika infections.
Perhaps most concerning is the absence of widespread RT-PCR testing, a technique that detects the active virus in blood or urine during the early phase of infection. Without RT-PCR testing, even symptomatic cases can go unconfirmed, leaving public health officials flying blind when it comes to tracking Zika’s spread.
Why Surveillance and Testing Matter
Preventing Congenital Defects
Pregnant women infected with Zika are at risk of giving birth to children with microcephaly and other developmental issues. Without testing, these risks go unnoticed.
Avoiding a Delayed Outbreak
Without real-time data, an outbreak may only be recognized after it spirals out of control—like dengue outbreaks in recent years.
Informing Policy and Resource Allocation
Evidence-based policymaking requires data. Without surveillance, resources can’t be allocated for mosquito control or public awareness campaigns.
What Bangladesh Needs to Do Now
To prevent a potential Zika outbreak and ensure early detection, Bangladesh must act proactively. The country already deals with mosquito-borne diseases like dengue and chikungunya, so the foundation for Zika preparedness exists—it just needs to be expanded thoughtfully. Here’s what must be done:
1. Integrate Zika Testing into Existing Dengue Programs
Bangladesh has an established network for dengue surveillance. By introducing Zika virus testing—particularly using multiplex diagnostic kits that can identify dengue, chikungunya, and Zika from the same sample—the country can enhance its disease detection capacity without building a whole new system. This integration will make early diagnosis faster, cheaper, and more accessible in both urban and rural areas.
2. Enhance Vector Control
Since Zika is spread by the same Aedes mosquitoes that transmit dengue, reinforcing vector control strategies can address all three viruses at once. Control efforts must be sustained year-round, not just during dengue season. This includes targeted larvicide application, regular clearing of stagnant water, improved waste management, and public campaigns promoting clean surroundings. Active participation from local governments and communities is essential for success.
3. Protect Pregnant Women
Pregnant women face the most serious consequences of Zika due to the risk of congenital Zika syndrome, including microcephaly in newborns. Bangladesh should develop special guidelines to screen pregnant women who show symptoms such as fever, rash, or joint pain—especially in high-risk areas. Health facilities must be trained to provide counseling, diagnostics, and proper monitoring for both the mother and child.
4. Build Public Awareness
A major gap in Zika preparedness is low public awareness. People need to understand how the virus spreads, how to prevent mosquito bites, and when to seek medical help. Information campaigns using television, radio, social media, and community health workers should focus on key messages such as:
-
Using mosquito repellents and bed nets
-
Covering water containers and removing standing water
-
Going to the doctor if symptoms arise, especially during pregnancy
5. Collaborate with Global Health Partners
Tackling Zika is not a task Bangladesh can manage alone. The country should strengthen partnerships with international health bodies such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC). Cooperation with neighboring countries—especially India, where Zika outbreaks have occurred—can help share data, surveillance techniques, and access to diagnostic tools. This kind of regional cooperation will be crucial in keeping Zika at bay.
Zika may not be making headlines in Bangladesh right now—but that doesn’t mean it isn’t here. The silent nature of the virus, combined with Bangladesh’s environmental vulnerabilities, makes it imperative to act before an outbreak happens. Surveillance, accurate testing, and informed policymaking are not optional—they’re essential. As the country continues to grapple with dengue and other mosquito-borne illnesses, the time to act on Zika is now—not later.
If you or someone you know is pregnant and experiencing fever or rash, consult a healthcare provider immediately. Demand testing. Awareness saves lives.
While Zika grabs headlines, waterborne illnesses like diarrhea and cholera quietly affect thousands. Stay informed and protected this season—read more here: https://inside-bangladesh.com/monsoon-disease-staying-safe-from-waterborne-illnesses